Page 381 - Cardiac Nursing
P. 381
1
1
1
/09
/09
/09
6 A
M
M
2:1
2:1
6 A
/30
87.
q
q
3-3
3-3
87.
6
6
/30
q
xd
xd
Pa
t
ara
ara
p
p
t
In
c.
c.
a
a
In
p
g
g
e 3
Pa
Pa
g
57
A
A
e 3
57
57
K34
LWBK340-c16_
16_
0-c
33
LWB K34 0-c 16_ p p pp333-387.qxd 6/30/09 12:16 AM Page 357 Aptara Inc.
LWB
33
C HAPTER 1 6 / Arrhythmias and Conduction Disturbances 357
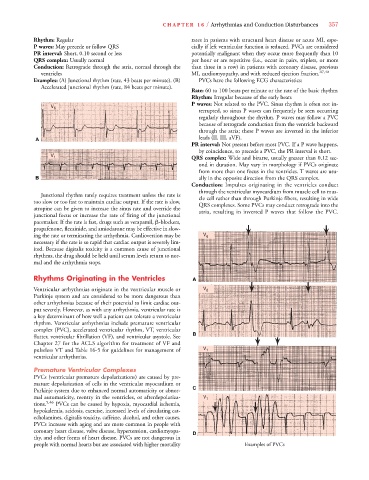
Rhythm: Regular rates in patients with structural heart disease or acute MI, espe-
P waves: May precede or follow QRS cially if left ventricular function is reduced. PVCs are considered
PR interval: Short, 0.10 second or less potentially malignant when they occur more frequently than 10
QRS complex: Usually normal per hour or are repetitive (i.e., occur in pairs, triplets, or more
Conduction: Retrograde through the atria, normal through the than three in a row) in patients with coronary disease, previous
ventricles MI, cardiomyopathy, and with reduced ejection fraction. 47,48
Examples: (A) Junctional rhythm (rate, 43 beats per minute). (B) PVCs have the following ECG characteristics:
Accelerated junctional rhythm (rate, 84 beats per minute).
Rate: 60 to 100 beats per minute or the rate of the basic rhythm
Rhythm: Irregular because of the early beats
P waves: Not related to the PVC. Sinus rhythm is often not in-
V 6
terrupted, so sinus P waves can frequently be seen occurring
regularly throughout the rhythm. P waves may follow a PVC
because of retrograde conduction from the ventricle backward
through the atria; these P waves are inverted in the inferior
A leads (II, III, aVF).
PR interval: Not present before most PVC. If a P wave happens,
by coincidence, to precede a PVC, the PR interval is short.
V 1 QRS complex: Wide and bizarre, usually greater than 0.12 sec-
ond in duration. May vary in morphology if PVCs originate
from more than one focus in the ventricles. T waves are usu-
B ally in the opposite direction from the QRS complex.
Conduction: Impulses originating in the ventricles conduct
through the ventricular myocardium from muscle cell to mus-
Junctional rhythm rarely requires treatment unless the rate is cle cell rather than through Purkinje fibers, resulting in wide
too slow or too fast to maintain cardiac output. If the rate is slow, QRS complexes. Some PVCs may conduct retrograde into the
atropine can be given to increase the sinus rate and override the atria, resulting in inverted P waves that follow the PVC.
junctional focus or increase the rate of firing of the junctional
pacemaker. If the rate is fast, drugs such as verapamil, -blockers,
propafenone, flecainide, and amiodarone may be effective in slow-
ing the rate or terminating the arrhythmia. Cardioversion may be V 6
necessary if the rate is so rapid that cardiac output is severely lim-
ited. Because digitalis toxicity is a common cause of junctional
rhythms, the drug should be held until serum levels return to nor-
mal and the arrhythmia stops.
Rhythms Originating in the Ventricles A A
Ventricular arrhythmias originate in the ventricular muscle or V 6
Purkinje system and are considered to be more dangerous than
other arrhythmias because of their potential to limit cardiac out-
put severely. However, as with any arrhythmia, ventricular rate is
a key determinant of how well a patient can tolerate a ventricular
rhythm. Ventricular arrhythmias include premature ventricular
complex (PVC), accelerated ventricular rhythm, VT, ventricular
flutter, ventricular fibrillation (VF), and ventricular asystole. See B B
Chapter 27 for the ACLS algorithm for treatment of VF and
pulseless VT and Table 16-5 for guidelines for management of V 1
ventricular arrhythmias.
Premature Ventricular Complexes
PVCs (ventricular premature depolarizations) are caused by pre-
mature depolarization of cells in the ventricular myocardium or
Purkinje system due to enhanced normal automaticity or abnor- C C
mal automaticity, reentry in the ventricles, or afterdepolariza- V 1
tions. 5,46 PVCs can be caused by hypoxia, myocardial ischemia,
hypokalemia, acidosis, exercise, increased levels of circulating cat-
echolamines, digitalis toxicity, caffeine, alcohol, and other causes.
PVCs increase with aging and are more common in people with
coronary heart disease, valve disease, hypertension, cardiomyopa- D D
thy, and other forms of heart disease. PVCs are not dangerous in
people with normal hearts but are associated with higher mortality Examples of PVCs