Page 75 - Cardiac Nursing
P. 75
0/2
0/2
6/3
6/3
009
1
5:3
009
1
0
q
q
68.
68.
q
0
0
xd
xd
5:3
p
p
1 A
1 A
p
r
r
ta
ta
e 5
Pa
Pa
3
3
Pa
g
e 5
g
g
2-0
K34
0-c
02_
LWB K34 0-c 02_ p p pp042-068.qxd 06/30/2009 15:33 Page 51 Aptara a a
LWBK340-c02_
LWB
04
04
2-0
C HAPTER 2 / Systemic and Pulmonary Circulation and Oxygen Delivery 51
subtypes. The 1 -adrenergic receptors, which are now characterized
as subtypes 1A , 1B , and 1D , are located in arteries, arterioles, and
cutaneous and visceral veins. The 1A receptors are responsible for
vessel contraction. The 1B receptors are thought to contribute to
the maintenance ofbasal vascular tone and arterialblood pressure
in conscious animals and are sensitive to exogenous agonists.
Finally, the 1D receptors also play a role in vascular contraction,
although they have a lesser effect than the 1B receptors. 107
The 2 receptors, whichhave presynaptic and postsynaptic
functions, are characterized as 2A/D , 2B , and 2C . The 2A/D
and 2B receptors are present in large arteries but are located with
greater density on the terminal arterioles, which act as precapillary
sphincters to control the number of open capillaries and total cap-
illary bloodflow. The 2A/D receptors play the primary role in
vasoconstriction. 108,109 The 2B receptors also play a role in vaso-
constriction and may contribute to the onset ofhypertension. The
2C receptors are responsible for venoconstriction. 107,110
Whereas stimulation of the presynaptic 2 receptors inhibits
norepinephrine, stimulation of the postsynaptic 2 receptors lo-
cated on the vascular smooth muscle causes norepinephrine re-
lease and subsequent vasoconstriction. However, the 2 -mediated
vasoconstriction is attenuatedby the 2 presynaptic inhibition of
norepinephrine release. In addition, in contrast to 1 receptor
stimulation, the effect of norepinephrine on 2 in terminal arteri-
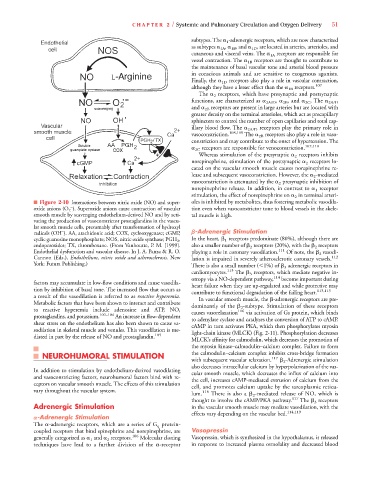
■ Figure 2-10 Interactions between nitric oxide (NO) and super- oles is inhibitedby metabolites, thus fostering metabolic vasodila-
–
oxide anions (O 2 ). Superoxide anions cause contraction of vascular tion even when vasoconstrictor tone to blood vessels in the skele-
smooth muscle by scavenging endothelium-derived NO and by acti- tal muscle is high.
vating the production of vasoconstrictor prostaglandins in the vascu-
lar smooth muscle cells, presumably after transformation of hydroxyl
–
radicals (OH ). AA, arachidonic acid; COX, cyclooxygenase; cGMP, -Adrenergic Stimulation
cyclic guanosine monophosphate; NOS, nitric oxide synthase; PGH 2 , In the heart, 1 receptors predominate (80%), although there are
endoperoxides; TX, thromboxane. (From Vanhoutte, P. M. [1999]. also a smaller number of 2 receptors (20%), with the 2 receptors
Endothelial dysfunction and vascular disease. In J. A. Panza & R. O. playing a role in coronary vasodilation. 111 Of note, the 2 vasodi-
Cannon (Eds.), Endothelium, nitric oxide and atherosclerosis. New lation is impaired in severely atherosclerotic coronary vessels. 112
York: Futura Publishing.) There is also a small number ( 1%) of 3 adrenergic receptors in
cardiomyocytes. 113 The 3 receptors, which mediate negative in-
otropy via a NO-dependent pathway, 114 become important during
factors may accumulate in low-flow conditions and cause vasodila- heart failure when they are up-regulated and while protective may
tion by inhibition of basal tone. The increased flow that occurs as contribute to functionaldegradation of the failingheart. 113,115
a result of the vasodilation is referred to as reactive hyperemia. In vascular smooth muscle, the -adrenergic receptors are pre-
Metabolic factors that have been shown to interact and contribute dominantly of the 2 -subtype. Stimulation of these receptors
to reactive hyperemia include adenosine and ATP, NO, causes vasorelaxation 116 via activation of Gs protein, whichbinds
prostaglandins, and potassium. 102–104 An increase in flow-dependent to adenylate cyclase and catalyzes the conversion of ATP to cAMP.
shear stress on the endothelium has also been shown to cause va- cAMP in turn activates PKA, which then phosphorylates myosin
sodilation in skeletal muscle and venules. This vasodilation is me- light-chain kinase (MLCK) (Fig. 2-11). Phosphorylation decreases
diated in part by the release of NO and prostaglandin. 105
MLCK’s affinity for calmodulin, whichdecreases the promotion of
the myosin kinase–calmodulin–calcium complex. Failure to form
NEUROHUMORAL STIMULATION the calmodulin–calcium complex inhibits cross-bridge formation
with subsequent vascular relaxation. 117 2 -Adrenergic stimulation
also decreases intracellular calcium by hyperpolarization of the vas-
In addition to stimulation by endothelium-derived vasodilating cular smooth muscle, whichdecreases the influx of calcium into
and vasoconstricting factors, neurohumoral factors bind with re- the cell, increases cAMP-mediated extrusion of calcium from the
ceptors on vascular smooth muscle. The effects of this stimulation cell, andpromotes calcium uptake by the sarcoplasmic reticu-
vary throughout the vascular system. 118
lum. There is also a 2 -mediated release of NO, which is
thought to involve the cAMP/PKA pathway. 117 The 3 receptors
Adrenergic Stimulation in the vascular smooth muscle may mediate vasodilation, with the
effects vary depending on the vascular bed. 114,119
-Adrenergic Stimulation
The -adrenergic receptors, which are a series of G q protein-
coupled receptors that bind epinephrine and norepinephrine, are Vasopressin
generally categorized as 1 and 2 receptors. 106 Molecular cloning Vasopressin, which is synthesized in the hypothalamus, is released
techniques have lead to a further division of the -receptor in response to increased plasma osmolality and decreased blood