Page 209 - ACCCN's Critical Care Nursing
P. 209
186 P R I N C I P L E S A N D P R A C T I C E O F C R I T I C A L C A R E
Ventricular chamber
pressure
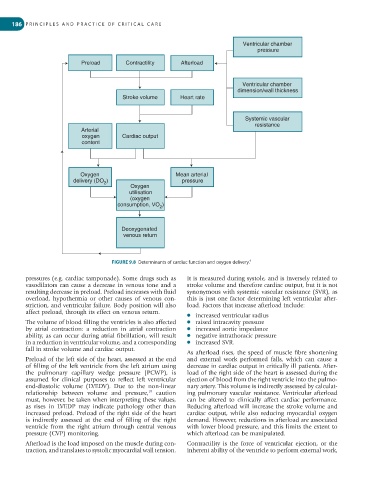
Preload Contractility Afterload
Ventricular chamber
dimension/wall thickness
Stroke volume Heart rate
Systemic vascular
resistance
Arterial
oxygen Cardiac output
content
Oxygen Mean arterial
delivery (DO ) pressure
2
Oxygen
utilisation
(oxygen
consumption, VO )
2
Deoxygenated
venous return
FIGURE 9.8 Determinants of cardiac function and oxygen delivery. 9
pressures (e.g. cardiac tamponade). Some drugs such as It is measured during systole, and is inversely related to
vasodilators can cause a decrease in venous tone and a stroke volume and therefore cardiac output, but it is not
resulting decrease in preload. Preload increases with fluid synonymous with systemic vascular resistance (SVR), as
overload, hypothermia or other causes of venous con- this is just one factor determining left ventricular after-
striction, and ventricular failure. Body position will also load. Factors that increase afterload include:
affect preload, through its effect on venous return.
● increased ventricular radius
The volume of blood filling the ventricles is also affected ● raised intracavity pressure
by atrial contraction: a reduction in atrial contraction ● increased aortic impedance
ability, as can occur during atrial fibrillation, will result ● negative intrathoracic pressure
in a reduction in ventricular volume, and a corresponding ● increased SVR.
fall in stroke volume and cardiac output.
As afterload rises, the speed of muscle fibre shortening
Preload of the left side of the heart, assessed at the end and external work performed falls, which can cause a
of filling of the left ventricle from the left atrium using decrease in cardiac output in critically ill patients. After-
the pulmonary capillary wedge pressure (PCWP), is load of the right side of the heart is assessed during the
assumed for clinical purposes to reflect left ventricular ejection of blood from the right ventricle into the pulmo-
end-diastolic volume (LVEDV). Due to the non-linear nary artery. This volume is indirectly assessed by calculat-
relationship between volume and pressure, caution ing pulmonary vascular resistance. Ventricular afterload
10
must, however, be taken when interpreting these values, can be altered to clinically affect cardiac performance.
as rises in LVEDP may indicate pathology other than Reducing afterload will increase the stroke volume and
increased preload. Preload of the right side of the heart cardiac output, while also reducing myocardial oxygen
is indirectly assessed at the end of filling of the right demand. However, reductions in afterload are associated
ventricle from the right atrium through central venous with lower blood pressure, and this limits the extent to
pressure (CVP) monitoring. which afterload can be manipulated.
Afterload is the load imposed on the muscle during con- Contractility is the force of ventricular ejection, or the
traction, and translates to systolic myocardial wall tension. inherent ability of the ventricle to perform external work,