Page 1764 - Williams Hematology ( PDFDrive )
P. 1764
1738 Part XI: Malignant Lymphoid Diseases Chapter 107: Myeloma 1739
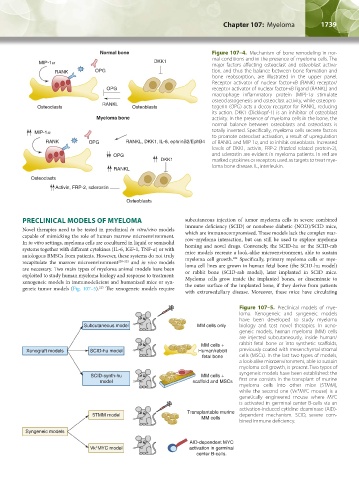
Normal bone Figure 107–4. Mechanism of bone remodeling in nor-
mal conditions and in the presence of myeloma cells. The
DKK1
major factors affecting osteoclast and osteoblast activa-
RANK OPG tion, and thus the balance between bone formation and
bone reabsorption, are illustrated in the upper panel.
Receptor activator of nuclear factor-κB (RANK) receptor/
OPG receptor activator of nuclear factor-κB ligand (RANKL) and
macrophage inflammatory protein (MIP)-1α stimulate
osteoclastogenesis and osteoclast activity, while osteopro-
RANKL
Osteoclasts Osteoblasts tegerin (OPG) acts a decoy receptor for RANKL, reducing
its action. DKK1 (Dickkopf-1) is an inhibitor of osteoblast
Myeloma bone activity. In the presence of myeloma cells in the bone, the
normal balance between osteoblasts and osteoclasts is
totally inverted. Specifically, myeloma cells secrete factors
to promote osteoclast activation, a result of upregulation
RANK OPG RANKL, DKK1, IL-6, ephrinB2/EphB4 of RANKL and MIP-1α, and to inhibit osteoblasts. Increased
levels of DKK1, activin, FRP-2 (frizzled related protein-2),
OPG and sclerostin are evident in myeloma patients. In red are
DKK1 marked cytokines or receptors used as targets to treat mye-
loma bone disease. IL, interleukin.
RANKL
Osteoclasts
Activin, FRP-2, sclerostin
Osteoblasts
PRECLINICAL MODELS OF MYELOMA subcutaneous injection of tumor myeloma cells in severe combined
Novel therapies need to be tested in preclinical in vitro/vivo models immune deficiency (SCID) or nonobese diabetic (NOD)/SCID mice,
which are immunocompromised. These models lack the complex mar-
capable of mimicking the role of human marrow microenvironment. row–myeloma interaction, but can still be used to explore myeloma
In in vitro settings, myeloma cells are cocultured in liquid or semisolid homing and novel drugs. Conversely, the SCID-hu or the SCID-rab
systems together with different cytokines (IL-6, IGF-1, TNF-α) or with mice models recreate a look-alike microenvironment, able to sustain
autologous BMSCs from patients. However, these systems do not truly myeloma cell growth. Specifically, primary myeloma cells or mye-
224
recapitulate the marrow microenvironment 220–222 and in vivo models loma cell lines are grown in human fetal bone (the SCID-hu model)
are necessary. Two main types of myeloma animal models have been or rabbit bone (SCID-rab model), later implanted in SCID mice.
exploited to study human myeloma biology and response to treatment: Myeloma cells grow inside the implanted bones, or disseminate to
xenogeneic models in immunodeficient and humanized mice or syn- the outer surface of the implanted bone, if they derive from patients
223
geneic tumor models (Fig. 107–5). The xenogeneic models require
with extramedullary disease. Moreover, these mice have circulating
Figure 107–5. Preclinical models of mye-
loma. Xenogeneic and syngeneic models
have been developed to study myeloma
Subcutaneous model MM cells only biology and test novel therapies. In xeno-
geneic models, human myeloma (MM) cells
are injected subcutaneously, inside human/
MM cells + rabbit fetal bone or into synthetic scaffolds,
Xenograft models SCID-hu model Human/rabbit previously coated with mesenchymal stromal
fetal bone cells (MSCs). In the last two types of models,
a look-alike microenvironment, able to sustain
myeloma cell growth, is present. Two types of
syngeneic models have been established: the
SCID-synth-hu MM cells +
model scaffold and MSCs first one consists in the transplant of murine
myeloma cells into other mice (5TMM),
while the second one (Vκ*MYC mouse) is a
genetically engineered mouse where MYC
is activated in germinal center B-cells via an
activation-induced cytidine deaminase (AID)-
Transplantable murine
5TMM model dependent mechanism. SCID, severe com-
MM cells
bined immune deficiency.
Syngeneic models
AID-dependent MYC
Vk*MYC model activation in germinal
center B-cells.
Kaushansky_chapter 107_p1733-1772.indd 1739 9/21/15 12:34 PM