Page 2144 - Williams Hematology ( PDFDrive )
P. 2144
2118 Part XII: Hemostasis and Thrombosis Chapter 123: Hemophilia A and Hemophilia B 2119
Pseudotumors (Blood Cysts)
Pseudotumors are blood cysts that occur in soft tissues or bone. They
are rare but dangerous complications of hemophilia (Fig. 123–10).
34
They are classified into three types. One type is a simple cyst that is con-
fined by tendinous attachments within the fascial envelope of a muscle.
The second type initially develops as a simple cyst in soft tissues such as
a tendon, but it interferes with the vascular supply to the adjacent bone
and periosteum, resulting in cyst formation and resorption of bone. The
third type is thought to result from subperiosteal bleeding that sepa-
rates the periosteum from the bony cortex. Most pseudotumors are not
associated with pain unless rapid growth or nerve compression occurs.
As the volume of the cyst increases, the cyst compresses and destroys
the adjacent muscle, nerve, and/or bone or expands around structures
A B like ureters causing renal failure. Pseudotumors usually contain either
Figure 123–7. A. A sagittal STIR (short tau inversion recovery) image serosanguineous fluid or a viscous brownish material surrounded by
of an ankle shows an effusion (white arrow). Edema in the distal tibia a fibrous membrane (Fig. 123–10). Pseudotumors have a tendency to
(asterisks) surrounds a debris-filled defect in the subchondral bone expand over several years and eventually become multiloculated. Some
of the distal tibia (black arrows). B. A coronal proton density of the ankle reach enormous size and involve so many structures that make them
in the same patient as in A shows the defect in the subchondral bone of inoperable. Erosion through surrounding tissues and penetration into
the distal tibia (white arrow). Mild narrowing of the tibiotalar joint (black
arrows) is more apparent laterally. viscera or through the skin can occur, usually as a late event. Sinus tracts
from the pseudotumor predispose to infection and septicemia. Pseu-
dotumors often develop in the lower half of the body, usually in the
thigh, buttock, or pelvis, but they can occur anywhere, including the
temporal bone. CT or MRI is useful for diagnosis. Needle biopsies of
pseudotumors should be avoided because of the risk of infection and
hemorrhage. A reliable treatment is operative removal of the entire
mass because the pseudotumor likely will reform if it is not completely
removed. Embolization, percutaneous drainage, and radiotherapy of a
pseudotumor have been reported and may be of value in hemophili-
acs with inhibitors when surgery is not possible. Surgical treatment
35
of patients with large pseudotumors should be done in a hemophilia
treatment center with a specialized multidisciplinary team of experts. 36
Hematuria
Many severely affected patients with hemophilia experience episodes of
spontaneous and asymptomatic hematuria. The urine may be brown or
red, depending upon the rate of bleeding. Most bleeding arises from
the renal pelvis, usually from one kidney but occasionally from both.
Appropriate studies to exclude a structural lesion in the kidneys should
be performed. Administration of factor replacement and hydration is
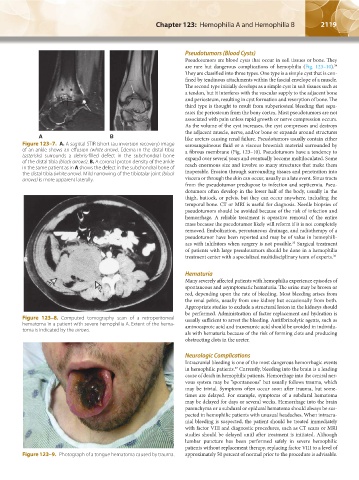
Figure 123–8. Computed tomography scan of a retroperitoneal usually sufficient to arrest the bleeding. Antifibrinolytic agents, such as
hematoma in a patient with severe hemophilia A. Extent of the hema- aminocaproic acid and tranexamic acid should be avoided in individu-
toma is indicated by the arrows.
als with hematuria because of the risk of forming clots and producing
obstructing clots in the ureter.
Neurologic Complications
Intracranial bleeding is one of the most dangerous hemorrhagic events
in hemophilic patients. Currently, bleeding into the brain is a leading
37
cause of death in hemophilic patients. Hemorrhage into the central ner-
vous system may be “spontaneous” but usually follows trauma, which
may be trivial. Symptoms often occur soon after trauma, but some-
times are delayed. For example, symptoms of a subdural hematoma
may be delayed for days or several weeks. Hemorrhage into the brain
parenchyma or a subdural or epidural hematoma should always be sus-
pected in hemophilic patients with unusual headaches. When intracra-
nial bleeding is suspected, the patient should be treated immediately
with factor VIII and diagnostic procedures, such as CT scans or MRI
studies should be delayed until after treatment is initiated. Although
lumbar puncture has been performed safely in severe hemophilic
patients without replacement therapy, replacing factor VIII to a level of
Figure 123–9. Photograph of a tongue hematoma caused by trauma. approximately 50 percent of normal prior to the procedure is advisable.
Kaushansky_chapter 123_p2113-2132.indd 2119 9/21/15 4:36 PM