Page 112 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 112
80 PART 1: An Overview of the Approach to and Organization of Critical Care
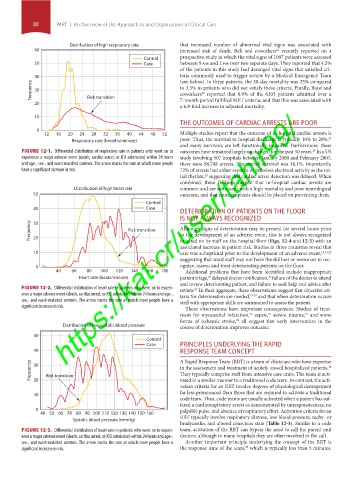
Distribution of high respiratory rate that increased number of abnormal vital signs was associated with
60 increased risk of death. Bell and coworkers recently reported on a
21
Control prospective study in which the vital signs of 1097 patients were assessed
50 Case between 9 am and 2 pm over two separate days. They reported that 4.5%
of the patients in this study had deranged vital signs that satisfied cri-
40 teria commonly used to trigger review by a Medical Emergency Team
(see below). In these patients, the 30-day mortality was 25% compared
Frequency 30 Risk transition to 3.5% in patients who did not satisfy these criteria. Finally, Buist and
coworkers reported that 8.9% of the 6303 patients admitted over a
22
20 7-month period fulfilled MET criteria, and that this was associated with
a 6.8-fold increase in adjusted mortality.
10
THE OUTCOMES OF CARDIAC ARRESTS ARE POOR
0 Multiple studies report that the outcome of in-hospital cardiac arrests is
12 16 20 24 28 32 36 40 44 48 52
23
Respiratory rate (breaths/minute) poor. Thus, the survival to hospital discharge is typically 10% to 20%,
and many survivors are left functionally impaired. Furthermore, these
FIGURE 12-1. Differential distribution of respiratory rate in patients who went on to outcomes have remained largely unchanged for the past 50 years. In a US
24
experience a major adverse event (death, cardiac arrest, or ICU admission) within 24 hours study involving 507 hospitals between January 2000 and February 2007,
and age-, sex-, and ward-matched controls. The arrow marks the rate at which more people there were 86,748 arrests. The overall survival was 18.1%. Importantly,
have a significant increase in risk. 72% of arrests had either asystole or pulseless electrical activity as the ini-
tial rhythm, suggesting that cardiac arrest detection was delayed. When
23
combined, these findings suggest that in-hospital cardiac arrests are
Distribution of high heart rate common and are associated with a high mortality and poor neurological
50 outcome, and that more emphasis should be placed on preventing them.
Control
40 Case
DETERIORATION OF PATIENTS ON THE FLOOR
IS NOT ALWAYS RECOGNIZED
Frequency 20 https://kat.cr/user/tahir99/
30
Although signs of deterioration may be present for several hours prior
Risk transition
to the development of an adverse event, this is not always recognized
or acted on by staff on the hospital floor (Figs. 12-4 and 12-5) with an
associated increase in patient risk. Studies in three countries reveal that
10 care was suboptimal prior to the development of an adverse event, 15,19,22
suggesting that ward staff may not have the skill set or resources to rec-
0 ognize, assess, and treat deteriorating patients on the floor.
40 60 80 100 120 140 160 180 Additional problems that have been identified include inappropriate
Heart rate (beats/minute) patient triage, delayed doctor notification, failure of the doctor to attend
25
26
and review deteriorating patient, and failure to seek help and advice after
FIGURE 12-2. Differential distribution of heart rate in patients who went on to experi- review. In their aggregate, these observations suggest that objective cri-
27
ence a major adverse event (death, cardiac arrest, or ICU admission) within 24 hours and age-, teria for deterioration are needed, 27-29 and that when deterioration occurs
sex-, and ward-matched controls. The arrow marks the rate at which more people have a staff with appropriate skills are summoned to assess the patient.
significant increase in risk.
These observations have important consequences. Studies of treat-
ment for myocardial infarction, sepsis, severe trauma, and some
30
32
31
forms of ischemic stroke, all suggest that early intervention in the
33
Distribution of low systolic blood pressure course of deterioration improves outcome.
50
Control
Case PRINCIPLES UNDERLYING THE RAPID
40 RESPONSE TEAM CONCEPT
Frequency 30 Risk transition A Rapid Response Team (RRT) is a team of clinicians who have expertise
in the assessment and treatment of acutely unwell hospitalized patients.
34
They typically comprise staff from intensive care units. The team is acti-
vated in a similar manner to a traditional code team. In contrast, the acti-
20
vation criteria for an RRT involve degrees of physiological derangement
far less pronounced than those that are required to activate a traditional
10
code team. Thus, code teams are usually activated when a patient has suf-
fered a cardiorespiratory arrest as demonstrated by unresponsiveness, no
0 palpable pulse, and absence of respiratory effort. Activation criteria for an
40 50 60 70 80 90 100110 120130 140150 160 RRT typically involve respiratory distress, low blood pressure, tachy- or
Systolic blood pressure (mmHg)
bradycardia, and altered conscious state (Table 12-3). Similar to a code
FIGURE 12-3. Differential distribution of heart rate in patients who went on to experi- team, activation of the RRT can bypass the need to call the parent unit
ence a major adverse event (death, cardiac arrest, or ICU admission) within 24 hours and age-, doctors, although in many hospitals they are often involved in the call.
sex-, and ward-matched controls. The arrow marks the rate at which more people have a Another important principle underlying the concept of the RRT is
35
significant increase in risk. the response time of the team, which is typically less than 5 minutes.
Section01.indd 80 1/22/2015 9:37:18 AM