Page 106 - The Netter Collection of Medical Illustrations - Integumentary System_ Volume 4 ( PDFDrive )
P. 106
Plate 4-21 Integumentary System
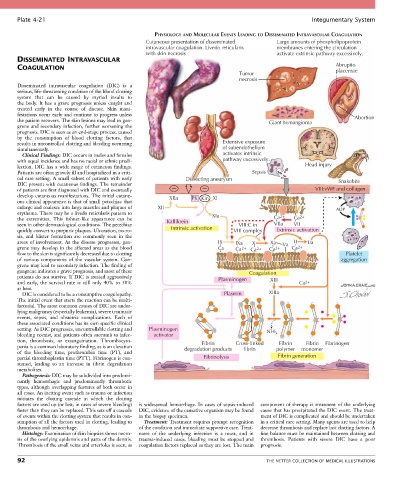
PHYSIOLOGY AND MOLECULAR EVENTS LEADING TO DISSEMINATED INTRAVASCULAR COAGULATION
Cutaneous presentation of disseminated Large amounts of phospholipoprotein
intravascular coagulation. Livedo reticularis membranes entering the circulation
with skin necrosis activate extrinsic pathway excessively.
DISSEMINATED INTRAVASCULAR
COAGULATION Abruptio
Tumor placentae
necrosis
Disseminated intravascular coagulation (DIC) is a
serious, life-threatening condition of the blood clotting
system that can be caused by myriad insults to
the body. It has a grave prognosis unless caught and
treated early in the course of disease. Skin mani-
festations occur early and continue to progress unless Abortion
the patient recovers. The skin lesions may lead to gan- Giant hemangioma
grene and secondary infection, further worsening the
prognosis. DIC is seen as an end-stage process, caused
by the consumption of blood clotting factors, that
results in uncontrolled clotting and bleeding occurring Extensive exposure
simultaneously. of subendothelium
Clinical Findings: DIC occurs in males and females activates intrinsic
with equal incidence and has no racial or ethnic predi- pathway excessively.
lection. DIC has a wide range of cutaneous findings. Head injury
Patients are often gravely ill and hospitalized in a criti- Sepsis
cal care setting. A small subset of patients with early Dissecting aneurysm Snakebite
DIC present with cutaneous findings. The remainder
of patients are first diagnosed with DIC and eventually VIII:vWF and collagen
develop cutaneous manifestations. The initial cutane- XIIa PK Kin XI
ous clinical appearance is that of small petechiae that
enlarge and coalesce into large macules and plaques of XII ADP
erythema. There may be a livedo reticularis pattern to XIa
the extremities. This fishnet-like appearance can be Kallikrein Ca 2+ Ca 2+
seen in other dermatological conditions. The petechiae VIII:C in VIIa VII
quickly convert to purpuric plaques. Ulceration, necro- Intrinsic activation VIII complex Extrinsic activation
sis, and blister formation are commonly seen in the
areas of involvement. As the disease progresses, gan- IX IXa X Xa Va II IIa
grene may develop in the affected areas as the blood Ca Ca Ca 2+ Ca 2+ Ca 2+
2+
flow to the skin is significantly decreased due to clotting Platelet
of various components of the vascular system. Gan- aggregation
grene may lead to secondary infection. The finding of
gangrene indicates a grave prognosis, and most of these Coagulation
patients do not survive. If DIC is treated aggressively Plasminogen XIII
and early, the survival rate is still only 40% to 50% Ca 2+
at best.
DIC is considered to be a consumptive coagulopathy. Plasmin XIIIa
The initial event that starts the reaction can be multi-
factorial. The most common causes of DIC are under-
lying malignancy (especially leukemia), severe traumatic
events, sepsis, and obstetric complications. Each of
these associated conditions has its own specific clinical
setting. As DIC progresses, uncontrollable clotting and Plasminogen NH
bleeding coexist, and patients often succumb to infec- activator 3
tion, thrombosis, or exsanguination. Thrombocyto- Fibrin Cross-linked Fibrin Fibrin Fibrinogen
penia is a common laboratory finding, as is an elevation degradation products fibrin polymer monomer
of the bleeding time, prothrombin time (PT), and
partial thromboplastin time (PTT). Fibrinogen is con- Fibrinolysis Fibrin generation
sumed, leading to an increase in fibrin degradation
metabolites.
Pathogenesis: DIC may be subdivided into predomi-
nantly hemorrhagic and predominantly thrombotic
types, although overlapping features of both occur in
all cases. An inciting event such as trauma or infection
initiates the clotting cascade in which the clotting
factors are used up (or lost, in cases of severe bleeding) is widespread hemorrhage. In cases of sepsis-induced component of therapy is treatment of the underlying
faster than they can be replaced. This sets off a cascade DIC, evidence of the causative organism may be found cause that has precipitated the DIC event. The treat-
of events within the clotting system that results in con- in the biopsy specimen. ment of DIC is complicated and should be undertaken
sumption of all the factors used in clotting, leading to Treatment: Treatment requires prompt recognition in a critical care setting. Many agents are used to help
thrombosis and hemorrhage. of the condition and immediate supportive care. Treat- decrease thrombosis and replace lost clotting factors. A
Histology: Examination of skin biopsies shows necro- ment of the underlying infection is a must, and in fine balance must be maintained between clotting and
sis of the overlying epidermis and parts of the dermis. trauma-induced cases, bleeding must be stopped and thrombosis. Patients with severe DIC have a poor
Thrombosis of the small veins and arterioles is seen, as coagulation factors replaced as they are lost. The main prognosis.
92 THE NETTER COLLECTION OF MEDICAL ILLUSTRATIONS