Page 112 - The Netter Collection of Medical Illustrations - Integumentary System_ Volume 4 ( PDFDrive )
P. 112
Plate 4-27 Integumentary System
ERYTHEMA MULTIFORME, STEVENS-JOHNSON SYNDROME, AND TOXIC EPIDERMAL NECROLYSIS
ERYTHEMA MULTIFORME,
STEVENS-JOHNSON SYNDROME,
AND TOXIC EPIDERMAL
NECROLYSIS
Erythema multiforme minor, erythema multiforme
major, Stevens-Johnson syndrome (SJS), and toxic epi-
dermal necrolysis are all classified as hypersensitivity
reactions, with the most common initiating event being
a medication or an infection. Some authors consider
these to be completely distinct entities with specific
etiologies. Until that is proven, a simple way of
approaching these diseases is to consider them as rep-
resenting a continuum with varying degrees of muco-
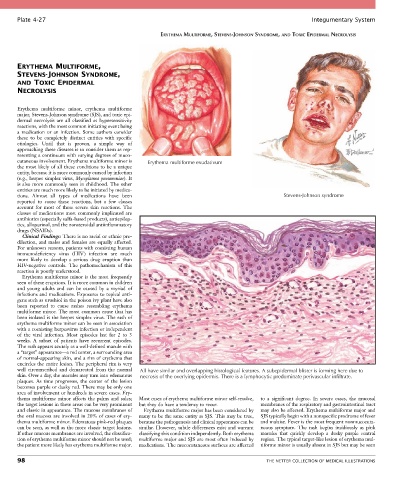
cutaneous involvement. Erythema multiforme minor is Erythema multiforme exudativum
the most likely of all these conditions to be a unique
entity, because it is more commonly caused by infection
(e.g., herpes simplex virus, Mycoplasma pneumoniae). It
is also more commonly seen in childhood. The other
entities are much more likely to be initiated by medica-
tions. Almost all types of medications have been Stevens-Johnson syndrome
reported to cause these reactions, but a few classes
account for most of these severe skin reactions. The
classes of medications most commonly implicated are
antibiotics (especially sulfa-based products), antiepilep-
tics, allopurinol, and the nonsteroidal antiinflammatory
drugs (NSAIDs).
Clinical Findings: There is no racial or ethnic pre-
dilection, and males and females are equally affected.
For unknown reasons, patients with coexisting human
immunodeficiency virus (HIV) infection are much
more likely to develop a serious drug eruption than
HIV-negative controls. The pathomechanism of this
reaction is poorly understood.
Erythema multiforme minor is the most frequently
seen of these eruptions. It is more common in children
and young adults and can be caused by a myriad of
infections and medications. Exposures to topical anti-
gens such as urushiol in the poison ivy plant have also
been reported to cause rashes resembling erythema
multiforme minor. The most common cause that has
been isolated is the herpes simplex virus. The rash of
erythema multiforme minor can be seen in association
with a coexisting herpesvirus infection or independent
of the viral infection. Most episodes last for 2 to 3
weeks. A subset of patients have recurrent episodes.
The rash appears acutely as a well-defined macule with
a “target” appearance—a red center, a surrounding area
of normal-appearing skin, and a rim of erythema that
encircles the entire lesion. The peripheral rim is very
well circumscribed and demarcated from the normal All have similar and overlapping histological features. A subepidermal blister is forming here due to
skin. Over a day, the macules may turn into edematous necrosis of the overlying epidermis. There is a lymphocytic predominate perivascular infiltrate.
plaques. As time progresses, the center of the lesion
becomes purple or dusky red. There may be only one
area of involvement or hundreds in severe cases. Ery-
thema multiforme minor affects the palms and soles; Most cases of erythema multiforme minor self-resolve, to a significant degree. In severe cases, the mucosal
the target lesions in these areas can be very prominent but they do have a tendency to recur. membranes of the respiratory and gastrointestinal tract
and classic in appearance. The mucous membranes of Erythema multiforme major has been considered by may also be affected. Erythema multiforme major and
the oral mucosa are involved in 20% of cases of ery- many to be the same entity as SJS. This may be true, SJS typically begin with a nonspecific prodrome of fever
thema multiforme minor. Edematous pink-red plaques because the pathogenesis and clinical appearance can be and malaise. Fever is the most frequent nonmucocuta-
can be seen, as well as the more classic target lesions. similar. However, subtle differences exist and warrant neous symptom. The rash begins insidiously as pink
If other mucous membranes are involved, the classifica- classifying this condition independently. Both erythema macules that quickly develop a dusky purple central
tion of erythema multiforme minor should not be used; multiforme major and SJS are most often induced by region. The typical target-like lesion of erythema mul-
the patient more likely has erythema multiforme major. medications. The mucocutaneous surfaces are affected tiforme minor is usually absent in SJS but may be seen
98 THE NETTER COLLECTION OF MEDICAL ILLUSTRATIONS