Page 184 - The Netter Collection of Medical Illustrations - Integumentary System_ Volume 4 ( PDFDrive )
P. 184
Plate 6-9 Integumentary System
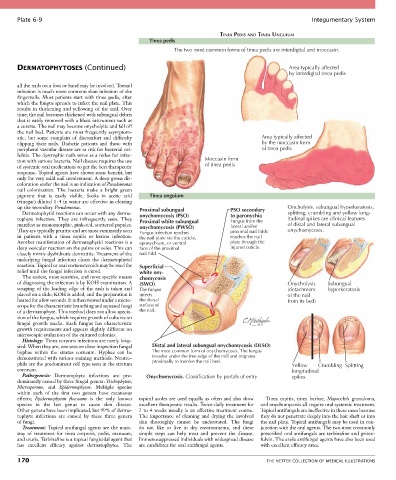
TINEA PEDIS AND TINEA UNGUIUM
Tinea pedis
The two most common forms of tinea pedis are interdigital and moccasin.
DERMATOPHYTOSES (Continued) Area typically affected
by interdigital tinea pedis
all the nails on a foot or hand may be involved. Toenail
infection is much more common than infection of the
fingernails. Most patients start with tinea pedis, after
which the fungus spreads to infect the nail plate. This
results in thickening and yellowing of the nail. Over
time, the nail becomes thickened with subungual debris
that is easily removed with a blunt instrument such as
a curette. The nail may become onycholytic and fall off
the nail bed. Patients are most frequently asymptom-
atic, but some complain of discomfort and difficulty Area typically affected
clipping their nails. Diabetic patients and those with by the moccasin form
peripheral vascular disease are at risk for bacterial cel- of tinea pedis
lulitis. The dystrophic nails serve as a nidus for infec-
tion with various bacteria. Nail disease requires the use Moccasin form
of systemic oral medications to get the best therapeutic of tinea pedis
response. Topical agents have shown some benefit, but
only for very mild nail involvement. A deep green dis-
coloration under the nail is an indication of Pseudomonas
nail colonization. The bacteria make a bright green
pigment that is easily visible. Soaks in acetic acid Tinea unguium
(vinegar) diluted 1 : 4 in water are effective in clearing
up the secondary Pseudomonas. Proximal subungual PSO secondary Oncholysis, subungual hyperkeratosis,
Dermatophytid reactions can occur with any derma- splitting, crumbling and yellow long-
tophyte infection. They are infrequently seen. They onychomycosis (PSO) to paronychia itudinal spikes are clinical features
Fungus from the
Proximal white subungual
manifest as monomorphic, pink-red, scattered papules. onychomycosis (PWSO) lateral and/or of distal and lateral subungual
They are typically pruritic and are most commonly seen Fungus infection reaches proximal nail folds onychomycosis.
in patients with a tinea capitis or kerion infection. the nail plate via the cuticle, reaches the nail
Another manifestation of dermatophytid reactions is a eponychium, or ventral plate through the
deep vesicular reaction on the palms or soles. This can face of the proximal injured cuticle.
closely mimic dyshidrotic dermatitis. Treatment of the nail fold.
underlying fungal infection clears the dermatophytid
reaction. Topical or oral corticosteroids may be used for Superficial
relief until the fungal infection is cured. white ony-
The easiest, most sensitive, and most specific means chomycosis
of diagnosing the infection is by KOH examination. A (SWO) Onycholysis Subungual
scraping of the leading edge of the rash is taken and The fungus (detachment hyperkeratosis
placed on a slide; KOH is added, and the preparation is infects of the nail
heated for a few seconds. It is then viewed under a micro- the dorsal from its bed)
scope for the characteristic branching and septated fungi surface of
of a dermatophyte. This method does not allow specia- the nail.
tion of the fungus, which requires growth of cultures on
fungal growth media. Each fungus has characteristic
growth requirements and appears slightly different on
microscopic evaluation of the cultured colonies.
Histology: Tinea corporis infections are rarely biop-
sied. When they are, one sees on close inspection fungal Distal and lateral subungual onychomycosis (DLSO)
hyphae within the stratus corneum. Hyphae can be The most common form of onychomycosis. The fungus
demonstrated with various staining methods. Neutro- invades under the free edge of the nail and migrates
phils are the predominant cell type seen in the stratum proximally to involve the nail bed. Yellow Crumbling Splitting
corneum. longitudinal
Pathogenesis: Dermatophyte infections are pre- Onychomycosis. Classification by portals of entry spikes
dominantly caused by three fungal genera: Trichophyton,
Microsporum, and Epidermophyton. Multiple species
within each of the first two genera have cutaneous
effects; Epidermophyton floccosum is the only known topical azoles are used equally as often and also show Tinea capitis, tinea barbae, Majocchi’s granuloma,
species in the last genus to cause skin disease. excellent therapeutic results. Twice-daily treatment for and onychomycosis all require oral systemic treatment.
Other genera have been implicated, but 99% of derma- 2 to 4 weeks usually is an effective treatment course. Topical antifungals are ineffective in these cases because
tophyte infections are caused by these three genera The importance of cleaning and drying the involved they do not penetrate deeply into the hair shaft or into
of fungi. skin thoroughly cannot be understated. The fungi the nail plate. Topical antifungals may be used in con-
Treatment: Topical antifungal agents are the main- do not like to live in dry environments, and these junction with the oral agents. The two most commonly
stay of treatment for tinea corporis, pedis, manuum, simple steps can help treat and prevent the disease. prescribed oral antifungals are terbinafine and griseo-
and cruris. Terbinafine is a topical fungicidal agent that Immunosuppressed individuals with widespread disease fulvin. The azole antifungal agents have also been used
has excellent efficacy against dermatophytes. The are candidates for oral antifungal agents. with excellent efficacy rates.
170 THE NETTER COLLECTION OF MEDICAL ILLUSTRATIONS