Page 502 - Cardiac Nursing
P. 502
LWBK340-c21_p460-510.qxd 09/09/2009 08:28 AM Page 478 Aptara
478 PA R T III / Assessment of Heart Disease
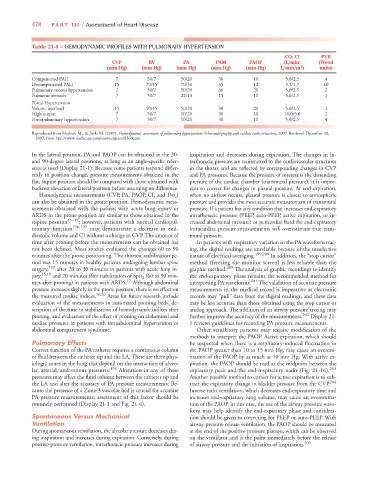
Table 21-4 ■ HEMODYNAMIC PROFILES WITH PULMONARY HYPERTENSION
CO; CI PVR
CVP RV PA PAM PAOP (L/min; (Wood
2 2 2
(mm Hg) (mm Hg) (mm Hg) (mm Hg) (mm Hg) L/min/m ) units)
Compensated PAH 7 50/7 50/20 30 10 5.0/2.5 4
Decompensated PAH 15 70/15 70/30 45 12 3.3/1.7 10
Pulmonary venous hypertension 7 50/7 50/20 30 20 5.0/2.5 2
Pulmonic stenosis 7 50/7 22/10 15 10 5.0/2.5 1
Portal Hypertension
Volume overload 15 50/15 50/20 30 20 5.0/2.5 2
High output 7 50/7 50/20 30 10 10.0/5.0 2
Portopulmonary hypertension 7 50/7 50/20 30 10 5.0/2.5 4
7
Reproduced from Mathier, M., & Park, M. (2007). Hemodynamic assessment of pulmonary hypertension: Echocardiography and cardiac catheterization, 2007. Retrieved December 28,
7
2007, from http://www.medscape.com/viewprogram/8360_pnt.
In the lateral position, PA and PAOP can be obtained in the 30- inspiration and decreases during expiration. The changes in in-
and 90-degree lateral positions, as long as an angle-specific refer- trathoracic pressure are transmitted to the cardiovascular structures
ence is used (Display 21-1). Because some patients respond differ- in the thorax and are reflected by corresponding changes in CVP
ently to position change, pressure measurements obtained in the and PA pressures. Because the pressure of interest is the distending
flat, supine position should be compared with those obtained with pressure of the cardiac chamber (transmural pressure), it is impor-
backrest elevation or lateral position before assuming no difference. tant to correct for changes in pleural pressure. At end-expiration,
Hemodynamic measurements (CVP, PA, PAOP, CI, and ) when no airflow occurs, pleural pressure is closest to atmospheric
can also be obtained in the prone position. Hemodynamic meas- pressure and provides the most accurate measurement of transmural
urements obtained with the patient with acute lung injury or pressure. If a patient has any condition that increases end-expiratory
ARDS in the prone position are similar to those obtained in the intrathoracic pressure (PEEP, auto-PEEP, active expiration, or in-
supine position 15–19 ; however, patients with normal cardiopul- creased abdominal pressure) or pericardial fluid the end-expiratory
monary function 196,197 may demonstrate a decrease in end- intracardiac pressure measurements will overestimate true trans-
diastolic volume and CI without a change in CVP. The amount of mural pressure.
time after proning before the measurements can be obtained has In patients with respiratory variation in the PA waveform trac-
not been defined. Most studies evaluated the changes 60 to 90 ing, the digital readings are unreliable because of the unselective
minutes after the prone positioning. The shortest stabilization pe- nature of electrical averaging. 199,200 In addition, the “stop cursor”
riod was 15 minutes in healthy patients undergoing lumbar spine method (freezing the monitor screen) is less reliable than the
surgery, 197 after 20 to 30 minutes in patients with acute lung in- graphic method. 200 The analysis of graphic recordings to identify
jury, 15,19 and 20 minutes after stabilization of SpO 2 (60 to 90 min- the end-expiratory phase remains the recommended method for
utes after proning) in patients with ARDS. 17 Although abdominal interpreting PA waveforms. 201 The validation of accurate pressure
pressure increases slightly in the prone position, there is no effect on measurements in the medical record is imperative as electronic
the measured cardiac indices. 16,20 Areas for future research include records may “pull” data from the digital readings, and these data
evaluation of the measurements in automated proning beds, de- may be less accurate than those obtained using the stop cursor or
scription of the time to stabilization of hemodynamic indices after analog approach. The addition of an airway pressure tracing may
proning, and evaluation of the effect of proning on abdominal and further improve the accuracy of the measurements. 202 Display 21-
cardiac pressures in patients with intraabdominal hypertension or 1 reviews guidelines for recording PA pressure measurements.
abdominal compartment syndrome. Other ventilatory patterns may require modification of the
methods to interpret the PAOP. Active expiration, which should
Pulmonary Effects be suspected when there is a respiratory-induced fluctuation in
Correct function of the PA catheter requires a continuous column the PAOP greater than 10 to 15 mm Hg, may cause an overesti-
of fluid between the catheter tip and the LA. There are three phys- mation of the PAOP by as much as 10 mm Hg. With active ex-
iologic zones in the lung that depend on the interaction of alveo- piration, the PAOP should be read at the midpoint between the
lar, arterial, and venous pressures. 198 Alteration in any of these expiratory peak and the end-inspiratory nadir (Fig. 21-16). 203
pressures may affect the fluid column between the catheter tip and Another possible method to correct for active expiration is to sub-
the LA and alter the accuracy of PA pressure measurements. Be- tract the expiratory change in bladder pressure from the CVP . 204
cause the presence of a Zone-3 vascular bed is crucial for accurate Inverse ratio ventilation, which decreases end-expiratory time and
PA pressure measurements, assessment of this factor should be increases end-expiratory lung volume, may cause an overestima-
routinely performed (Display 21-1 and Fig. 21-4). tion of the PAOP. In this case, the use of the airway pressure wave-
form may help identify the end-expiratory phase and considera-
Spontaneous Versus Mechanical tion should be given to correcting for PEEP or auto-PEEP. With
Ventilation airway pressure release ventilation, the PAOP should be measured
During spontaneous ventilation, the alveolar pressure decreases dur- at the end of the positive pressure plateau, which can be observed
ing inspiration and increases during expiration. Conversely, during on the ventilator and is the point immediately before the release
positive-pressure ventilation, intrathoracic pressure increases during of airway pressure and the initiation of inspiration. 205